Procedures. Emergency Department response on CBRNE incidents.
CBRNEmedicine Procedures. Emergency Department response on CBRNE incidents. Initial detection of radiation contamination and health ionising radiation consequences.
Arkadiusz Trzos1, Karol Łyziński1, Katarzyna Kącka2
1)Jagiellonian University Medical College, Faculty of Medicine, Chair of Anaesthesiology and Intensive Care, Department of Disaster Medicine and Emergency Care
2)Jagiellonian University Medical College, Faculty of Medicine, Chair of Anaesthesiology and Intensive Care, Department of Anaesthesiology and Intensive Care
Summary:
Possible escalation of military conflict in the Ukraine increases the risk of radiation-related incident in Europe. The use of tactical nuclear weapon, „dirty bomb” or damage to nuclear power plant may lead to radioactive contamination of terrain and people. The increased risk of hospital Emergency Department receiving patients exposed to radiation calls for preparing the emergency medical system and hospitals in advance. Department of Emergency and Disaster Medicine of the Jagiellonian University Medical College participates in creating medical procedures for handling CBRNE threat. This article presents proposed CBRNEmedicine procedures regarding initial treatment of CBRNE incident victim. Procedures cover in detail the initial detection and identification of the radiation source within the ED, method of assessing the scale of internal and external contamination, the amount of ionizing radiation absorbed (CBRNE point of care testing project), METREPOL radiation triage and the perspectives of using devices based on artificial intelligence capabilities.
Key words: CBRNE, ionizing radiation, medical response, detection, identification, triage
English version of the publication:

CBRNEmedicine procedures. Emergency Department response to CBRNE incidents. Initial detection of radiation contamination and ionizing radiation health consequences.
Introduction
Possible escalation of military conflict in the Ukraine brings an increased risk of using weapon of mass destruction (NBC/CBRNE) to achieve tactical and operational superiority [1], [2]. The use of tactical nuclear weapon or radioactive contamination (resulting from deliberate or accidental damage to nuclear power plant) or using a „dirty bomb” for military or terrorist purposes is possible. It calls for proper preparation of emergency medical system and healthcare system in Poland to respond the possible consequences of radiation or nuclear incidents.
One of the elements preparing for CBRNE threat is creating modern procedures for treating radiated or contaminated patient in the Emergency Department (ED), medical transfer points and field hospitals created for the sake of treating CBRNE incident casualties. Recent years have shown rapid development in clinical research concerning health results of radiation. It makes it necessary to keep medical treatment procedures updated [3]. The already known diagnostic methods are now broadened by the use of mobile detection and identification devices in the ED, along with implementing medical treatment [4].
Detecting contamination and fast identification of radioactive factor present on skin surface or within patient’s organism enable assessing the scale of exposure to radiation, effectiveness of decontamination, and eventually the scale of threat and potential outcome both for the patient and medical personnel.
Currently in Polish rescue system only the State Fire Service and the National Firefighting Rescue System are equipped with tools allowing rapid detection and identification of radioactive agents within human environment [5]. State Emergency Medical System currently has no tools allowing to detect and identify radioactive agents or other CBRNE threats. This concerns both the pre-hospital and ED level. Creating CBRNE-profile Rescue Task Force teams in Poland would change the situation. Specialist hospital clinical departments, such as toxicology, radiology or radiotherapy have tools allowing for detecting and identifying radioactive agents on skin or elsewhere within the patient’s organism. For example scintigraphy enables identification of places within the body where radionuclide accumulates. Facing war threat, the capability of fast detection of increased amount of ionizing radiation within the environment, including confirming patient’s contamination, will prove crucial in providing safety to medical personnel and increasing treatment effectiveness.
Department of Disaster and Emergency Medicine of the Jagiellonian University Collegium Medicum in Kraków committed to create new medical procedures of treating CBRNE incident casualties. This takes place within the Strengthening CBRNE safety and security – Coordination and Standardization project, financed by the 2014-2021 Norway Grants. Medical procedures, under the collective name CBRNEmedicine cover the rules of medical action on pre-hospital level (Emergency Medical Service Teams) and early in-hospital (Emergency Department). This publication describes selected CBRNEmedicine radiation procedures including early bedside radiation diagnostics, the CBRNE Point of Care Testing.
Emergency Department tasks after radiation incident
Tasks for the Emergency Department after radiation incident result directly from legal acts regulating the principles of emergency medical system functioning in Poland [6],[7]. Currently the organizational structure and equipment of Emergency Department allows for initial treatment of radiated patient, but without the early measurement of scale and type of radiation threat present. Each Emergency Department has proper and sufficient infrastructure, medical and decontamination devices and personal protective equipment (PPE) allowing for safe treatment of patient contaminated by radiation.
ED medical personnel’s task is to safely admit the patient, perform initial triage, secure the basic vital functions, complete the medical decontamination, perform broadened triage (including specialist, such as radiation-related), implement preventive measures and begin symptomatic treatment. The final stage in ED action chain is transport to proper clinical department or specialist hospital for definitive treatment. Currently, after radiation incident, personnel of ED has to grope their way in order to complete all the above-mentioned action, with no way to detect or identify the radioactive material. Without the support from State Fire Service or National Firefighting Rescue System there is currently no way ED staff can detect and identify radiation threats on their own.
CBRNEmedicine procedures recommend that in case of CBRNE threat, the medical personnel of ED should use the C-level protective gear, according to The Occupational Safety and Health Administration categories [8]–[11]. Procedures recommend to use full-face masks and combination filters with CBRNE certification as standard. Protective suits should meet the PN-EN 1073- 2:2005 standard. Filters and combination filters should meet the highest (III P3) class of PN-EN 143:2021 norm [9], [12], [13]. Because of chemical characteristics of radioactive substances multi-gas combination filters used should meet the PN-EN 14387:2021 standard (for example the AVEC NBC-3/SL M type A2B2E2K2HgSXP3 DR, dedicated for masks with Rd40 1/7’’ threaded socket, meeting the STANAG 4155 / PN-EN 148-1 standard). Individual equipment should contain Personal Electronic Dosimeters, which measure the dose-equivalent rate absorbed by the medical personnel (for example the Polimaster PM1610A, TracercoTM (PED) ER+, RadEye GN.)
Problem to solve
The main challenge faced by the ED medical personnel is the rapid detection of threat, its identification and further neutralization or removal. During direct contact with radioactive material the amount of ionizing radiation absorbed depends on the power of dose and exposure time. Therefore the moment of detecting radioactive contamination, along with the speed and quality of both external and internal decontamination, are decisive in terms of the scale of dose absorbed (both locally and for the whole organism). External contamination (skin, clothing, direct surrounding, personal belongings) are a secondary threat for medical personnel, other staff and in-hospital environment (ED). The method of detection and identification proposed by the CBRNEmedicine allows for rapid identification of radioactive threat.
CBRNE Point of Care Testing
CBRNE Point of Care Testing is a method allowing for fast track bedside diagnostics of hazardous agents, on each stage of treating CBRNE incident casualty. The method proposed may be implemented on scene, during evacuation and transport, in medical transfer points and hospitals, including field hospitals. The goal of CBRNE Point of Care Testing project is creating the rules of fast detection and identification of hazardous factors, determining the threat level and the amount of radiation absorbed or the risk of spreading the contamination. This will make it easier to triage patients, allowing to estimate the potential health outcome. Information gathered this way, processed by tools based on Artificial Intelligence technology will allow to create the optimal method of treating single patient and managing medical help in case of more casualties.
Detection and identification of radiation source
Detection and radiation identification method proposed in CBRNEmedicine procedures is based on detecting the presence of ionizing radiation in the environment with the use of stationary and mobile measurement tools. Locating radiation detectors outside and inside the ED, mainly by the entrance and in triage room, will enable fast-check of all the individuals entering the ED and detecting radiation threat in case of patient or EMS team unaware of hazard presence.
In further bedside treatment, CBRNEmedicine radiation procedures recommend the use of mobile devices.
Fot.1. Detection device used for CBRNE Point of Care Testing procedure.
(Source: authors’ archive, equipment: Raytech courtesy)

Fot.2. Detection device used for CBRNE Point of Care Testing procedure.
(Source: authors’ archive, equipment: Raytech courtesy)

Mobile devices enable in-depth scan of the whole skin surface and clothing, along with analyzing samples of secretion and discharge. Confirming the presence of external contamination allows for precise measurements on the skin in order to identify places of higher radiation level – the hot spots. Clear marking of those spots on skin drives attention towards them during decontamination. Measuring the radioactivity of secretion of foreign objects removed from body allows for detecting internal contamination.
Fot.3. CBRNE Point of Care Testing procedure radiation scanning of patient (simulation of radiation incident) (Source: authors’ archive, equipment: Raytech courtesy)

CBRNE Pre-triage and initial ABCDE triage
In the era of military threat authors of CBRNEmedicine procedures recommend the initial CBRNE pre-triage of all patients arriving from the hazardous zone. This enables detecting the presence of hazardous biological, chemical, radioactive and pyrotechnical materials. Devices currently available enable fast, bedside detection and identification of hazardous materials and performing differential diagnostics of CBRNE factors.
The next (or parallel) stage in CBRNEmedicine procedures is the initial clinical ABCDE triage based on assessing the basic vital signs: breathing, circulation, central nervous system and reasons of illness or injuries. The goal of CBRNE pre-triage and ABCDE initial triage is to determine the presence of threats critical for survival and to determine the amount and priority of particular (critical) medical life saving interventions, such as decontamination, cardiopulmonary resuscitation, selected surgical interventions, administering specific antidotes, etc. While the initial ABCDE triage determines the level of life threat and the need to perform critical interventions, the CBRNE pre-triage searches for the reasons of patient’s condition deterioration in the spectrum of hazardous materials influence. These both methods of initial assessment are complementary, and eventually create a single part of the proposed CBRNEmedicine procedures.
Medical decontamination
Decontamination process removes or neutralizes hazardous substance. In case of radiation incidents there is no way of neutralizing radioactive isotopes, these can only be removed from skin surface and from the body. CBRNEmedicine radiation procedures created predict the need of fast external and internal decontamination, in order to remove as much radioactive material detected as possible. Procedures agree that the initial external decontamination can be completed with specialist packages, enabling dry decontamination, such as DECPOL RAD® – Radiodecontamination wipes.
Fot.4. Dry decontamination in the field (simulation of radiation incident) (Source: authors’ archive)

Procedures recommend measuring the amount of initial and final radiation level, especially the spots with high radiation level read. On the base of this, the effectiveness of decontamination and the need to continue is assessed.
In order to initially decontaminate the airway, it is recommended to rinse the upper airway and bronchi with closed suction devices, along with taking a sample to assess contamination level. The recommended method of decontaminating gastrointestinal tract is administering activated carbon, which binds radioactive material and limits it absorption to blood-flow. At the same time digesta and vomit should be secured, in order to assess contamination level of the gastrointestinal tract. Forcing vomiting and gastric lavage is performed or not upon lead physician’s decision, based mainly on time since the exposure. In order to support decontamination process by limiting absorption and redistribution of isotopes in body tissue (vital organs) it is recommended to use chelating agents, such as iodine and Prussian blue, depending on the type of radioactive isotope recognized [14]. It is recommended to perform initial internal decontamination based on standard protocols of infusion fluid therapy along with administering neutralizing diuretics. Urine is to be subjected to radiation assessment.
Proper decontamination is a multi-level process of precise removal of hazardous material from the skin (external decontamination) and from within the organism (internal decontamination). Early external decontamination should be performed in decontamination chamber before entering the ED.
Fot.5. External decontamination in decontamination chamber (simulation of radiation incident) (Source: authors’ archive)

Further stages include deep cleaning of the contaminated spots, and can be completed on patient’s bed providing proper protection of ED environment and medical personnel.
CBRNEmedicine procedures recommend that proper internal decontamination – the attempt to rinse radioactive isotope from the organism – should be performed according to guidelines of clinical toxicology and kidney-dialysis therapy centers, with the use of dialysis in dedicated medical facilities.
It is recommended to continue external decontamination up until the moment when the result of measurement is no more than twice the background level (in decontamination location) or no more than 10% of the previous contamination level [15].
CBRNE Point of Care Testing bedside diagnostics enable assessing the level of internal contamination by measuring the radioactivity of physiological fluids, secretion and discharge of the organism and tissue samples from wounds. Following the dynamics of internal contamination level change enables to determine the effectiveness of decontamination and the purposefulness of continuing it. The method allows to determine, with the use of AI tools, the potential (early, deterministic) health outcome of exposure to ionizing radiation.
METREPOL radiation triage
In clinical action, CBRNEmedicine radiation procedure recommends the initial screening radiation triage aimed at determining the approximate amount of ionizing radiation dose absorbed. It should be based on clinical manifestation of primary response. Proper triage should be based on traditional METREPOL triage (MEdical TREatment ProtocOLs for Radiation Accident Victims) [16]–[18]
Fig. 1. METREPOL medical triage protocol [16], [17] [19]
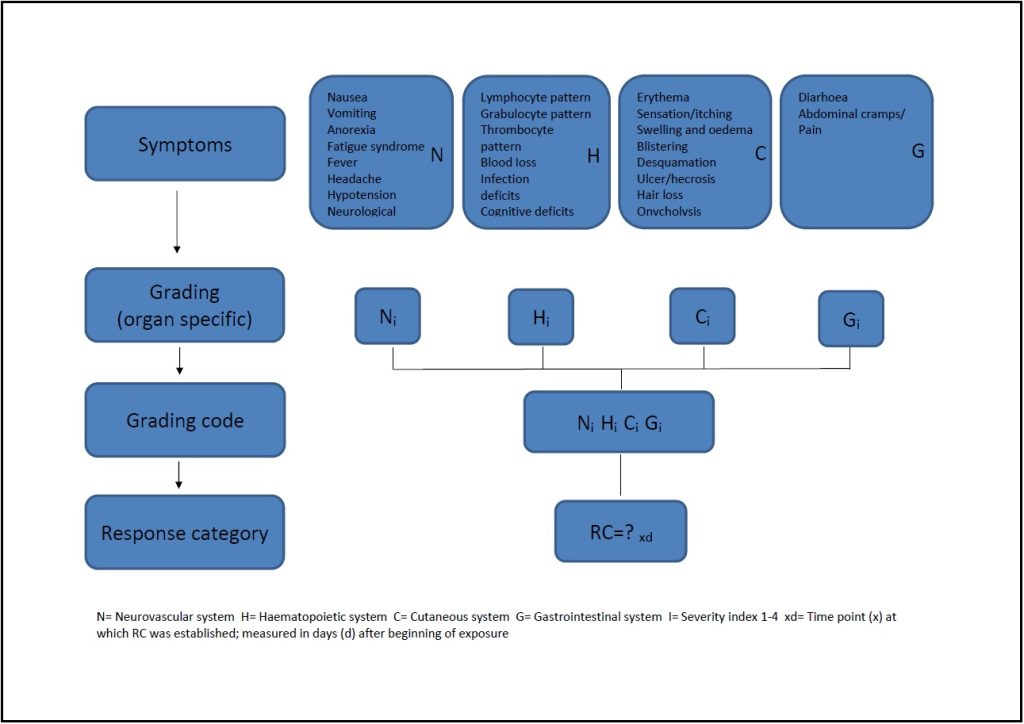
Assessment of intensity and the course of primary reaction is currently of limited use in single casualty incidents and incidents with several casualties. In case of mass casualty incidents and disasters, the value of this method increases, when information gathered from patients is incorporated into general database and processed by AI tools, allowing to make the process of managing medical help more effective [20].
In case of single- and many-casualty incidents, the efficient laboratory diagnostics in every case of illness enables employing laboratory diagnostic methods recommended by international standards [21],[9]. The basic test taken in the ED is the full blood morphology, allowing to determine the lymphocytes count and the dynamics of its change, and further – the effective dose absorbed by the organism [3], [9],[22].
Determining the effective dose enables to qualify the ED patient to adequate segregation group, predict the course of lesion, and eventually properly select the place and method of treatment and estimate the chance of survival depending on the place and proposed treatment.
Artificial Intelligence in the CBRNEmedicine project
The use of Artificial Intelligence is an integral part of CBRNEmedicine project. Technological challenge, which appears after radiation incident (CBRNE), is to integrate data from various sources, which allows monitoring patient’s health status. Effective management of treatment requires gathering information from official data sources (external and internal) and enriching them with data from open sources (Open Source Intelligence). This calls for using IT solution, capable of acquiring and processing data in various formats, incoming with variable frequency from heterogeneous sources. Traditional algorithms, based on time series, prove not useful in predicting events such as radiation incident (CBRNE) and its consequences, which requires the search for new, more effective AI solutions. Such solutions are more effective at optimizing diagnostic and therapeutic process, allocation and transport of patients, as well as the use of medical personnel and ED resources based on gathering and processing various data in real time. Algorithms strengthening gradient and artificial neural networks used for CBRNEmedicine project may prove very effective, as they properly tackle complex problems and provide good results even while working on incomplete data from various sources.
Conclusion
By making bedside detection and identification of CBRNE agents common, CBRNE point of care testing project will make it possible to quickly identify hazard on successive stages of medical action, and will become a source of data for medical care management system. Incorporating data gathered in this way and processing them with the use of solutions based on Artificial Intelligence algorithms broadens the capabilities of CBRNEmedicine project, making it an up-to-date tool in contemporary medical rescue.
References:
[1] “How to Avoid the Ukraine War Going Nuclear | Time.” https://time.com/6244330/russia-ukraine-war-nuclear-threat/ (accessed Feb. 10, 2023).
[2] “How will the Russia-Ukraine war reshape the world? Here are four possible futures. – Atlantic Council.” https://www.atlanticcouncil.org/content-series/the-big-story/how-will-the-russia-ukraine-war-reshape-the-world-here-are-four-possible-futures/ (accessed Feb. 10, 2023).
[3] M. C. Thorne, “Responding to radiation accidents: what more do we need to know?,” Journal of Radiological Protection, vol. 42, no. 3, Sep. 2022, doi: 10.1088/1361-6498/AC8C4C.
[4] A. Trzos, “Przygotowanie oddziału ratunkowego na zagrożenia CBRNiE/HAZMAT.,” in Ratownictwo medyczne wobec współczesnych zagrożeń., Katowice: Elamed Media Group, 2019, p. s. 297-312. [Online]. Available: https://zagrozenia-nar.elamed.pl/
[5] Artur Ankowski, Iwona Nowak-Maj, and Tomasz Golenowski, “Rozpoznanie czynników zagrożenia w zdarzeniach CBRNiE/HAZMAT,” in Ratownictwo medyczne wobec współczesnych zagrożeń, I., Katowice: Elamed, 2019, pp. 223–241.
[6] “Ustawa z dnia 8 września 2006 r. o Państwowym Ratownictwie Medycznym.” https://isap.sejm.gov.pl/isap.nsf/DocDetails.xsp?id=wdu20061911410 (accessed Aug. 19, 2022).
[7] Obwieszczenie Ministra zdrowia w sprawie ogłoszenia jednolitego tekstu rozporządzenia Ministra Zdrowia w sprawie szpitalnego oddziału ratunkowego.
[8] H. H. Tan, M. Leong, R. Ponampalam, C. Y. Lee, and J. Goh, “Hazmat Medical Life Support,” Hazmat Medical Life Support, Aug. 2014, doi: 10.1142/9076.
[9] C. Rojas-Palma et al., “Triage, Monitoring and Treatment of people exposed to ionising radiation following a malevolent act.” [Online]. Available: www.tmthandbook.org
[10] “OSHA BEST PRACTICES for HOSPITAL-BASED FIRST RECEIVERS OF VICTIMS from Mass Casualty Incidents Involving the Release of Hazardous Substances OSHA Best Practices for Hospital-based First Receivers,” 2005.
[11] K. L. Koenig and C. H. Schultz, Koenig and Schultz’s Disaster Medicine: Comprehensive Principles and Practices. Cambridge University Press, 2016. [Online]. Available: https://books.google.pl/books?id=zffUCwAAQBAJ
[12] K. Łyziński et al., “Ratownictwo medyczne wobec zagrożeń radiacyjnych-cz. 2. Postępowanie przedszpitalne PRM.” [Online]. Available: www.ratownicy24.pl
[13] A. Trzos, K. Łyziński, and K. Długosz, “Indywidualne środki ochrony dla ratownictwa medycznego.,” Na Ratunek, no. nr 4, p. s. 22-28, 2018, [Online]. Available: http://naratunek.elamed.pl/
[14] R. Acosta and S. J. Warrington, “Radiation Syndrome,” StatPearls, vol. 5, no. 5, pp. 277–283, Mar. 2022, Accessed: Feb. 10, 2023. [Online]. Available: https://www.ncbi.nlm.nih.gov/books/NBK441931/
[15] K. L. Koenig et al., “Medical treatment of radiological casualties: Current concepts,” Ann Emerg Med, vol. 45, no. 6, pp. 643–652, Jun. 2005, doi: 10.1016/J.ANNEMERGMED.2005.01.020.
[16] L. Lebaron-Jacobs and E. Herrera-Reyes, “The METREPOL criteria—are they still relevant?,” Journal of Radiological Protection, vol. 42, no. 1, p. 014003, Jan. 2022, doi: 10.1088/1361-6498/AC3BC2.
[17] T. M. Fliedner, R. Powles, B. Sirohi, D. Niederwieser, and on behalf of the E. G. for B. and M. T. (EBMT) N. A. C. (NAC), “Radiologic and nuclear events: the METREPOL severity of effect grading system,” Blood, vol. 111, no. 12, pp. 5757–5758, Jun. 2008, doi: 10.1182/BLOOD-2008-04-150243.
[18] I. Friesecke, K. Beyrer, and T. M. Fliedner, “How to cope with radiation accidents: the medical management,” Br J Radiol, vol. 74, no. 878, pp. 121–122, 2001, doi: 10.1259/BJR.74.878.740121.
[19] I. Friesecke, K. Beyrer, and T. M. Fliedner, “How to cope with radiation accidents: the medical management,” Br J Radiol, vol. 74, no. 878, pp. 121–122, 2001, doi: 10.1259/BJR.74.878.740121.
[20] J. T. Dant, G. Reeves, and D. Stricklin, “Automated Translation of Clinical Parameters in Evaluating Acute Radiation Injury: Results From a Mass Casualty Exercise,” Disaster Med Public Health Prep, vol. 12, no. 5, pp. 569–573, Oct. 2018, doi: 10.1017/DMP.2017.126.
[21] L. K. Wathen, P. S. Eder, G. Horwith, and R. L. Wallace, “Using biodosimetry to enhance the public health response to a nuclear incident,” https://doi.org/10.1080/09553002.2020.1820605, vol. 97, no. S1, pp. S6–S9, 2020, doi: 10.1080/09553002.2020.1820605.
[22] V. Nair, D. N. Karan, and C. S. Makhani, “Guidelines for medical management of nuclear/radiation emergencies,” Med J Armed Forces India, vol. 73, no. 4, p. 388, Oct. 2017, doi: 10.1016/J.MJAFI.2017.09.015.